“Comparative study showed that children faced a 78% higher risk of new‐onset conditions after they had COVID‐19”, Long Covid Research Roundup, February 4
Long Covid Research Roundup, February 4
Compilation taken from Sam Rhode’s post.
Long COVID impacting more than 1 million children: CDC study suggests - ABC News
Higher levels of long COVID were found in lower-income households.
Results of the analysis, published in the journal JAMA Pediatrics, showed approximately 1.01 million children, or 1.4%, are believed to have ever experienced long COVID in 2023 and about 293,000, or 0.4%, were experiencing the condition when the survey was being conducted.
Among children currently experiencing long COVID at the time of interview, 80% reported to have some level of activity limitation compared with before they had COVID-19.
Comparative study showed that children faced a 78% higher risk of new‐onset conditions after they had COVID‐19 - Di Chiara - 2023 - Acta Paediatrica - Wiley Online Library
Results: We compared 1656 exposed and 1656 unexposed children from 1 February 2020 to 30 November 2021. The overall excess risk for new-onset conditions after COVID-19 was 78% higher in the exposed than unexposed children. We found significantly higher risks for some new conditions in exposed children, including mental health issues (aHR 1.8, 95% CI 1.1-3.0) and neurological problems
Covid-19 ‘brain fog’ likely factor in near-miss train crash in South Island - NZ Herald
· A KiwiRail engineer experiencing after-effects of Covid-19 failed to stop at a red signal nearly causing a train collision last year.
· The engineer ran a red light at 44km/h but avoided a crash as track settings kept it on the main line.
· TAIC has warned of post-Covid cognitive issues affecting safety-critical workers.
“Medical advice received by the commission was that potential effects of Covid-19 on cognitive impairment [’brain fog’] are well documented and can be long-lasting, continuing after the infection has cleared,” the report said.
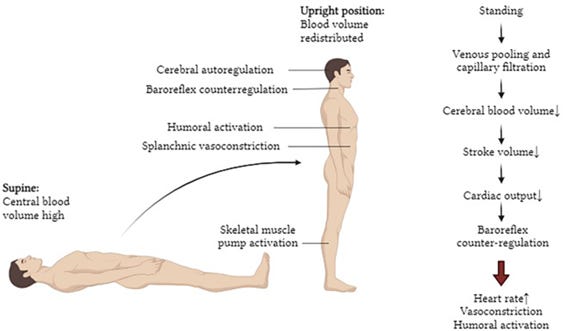
Cerebral Blood Flow in Orthostatic Intolerance | Journal of the American Heart Association
Cerebral blood flow (CBF) is vital for delivering oxygen and nutrients to the brain. Many forms of orthostatic intolerance (OI) involve impaired regulation of CBF in the upright posture, which results in disabling symptoms that decrease quality of life. Because CBF is not easy to measure, rises in heart rate or drops in blood pressure are used as proxies for abnormal CBF. These result in diagnoses such as postural orthostatic tachycardia syndrome and orthostatic hypotension. However, in many other Ol syndromes such as myalgic encephalomyelitis/chronic fatigue syndrome and long COVID, heart rate and blood pressure are frequently normal despite significant drops in CBF. This often leads to the incorrect conclusion that there is nothing hemodynamically abnormal in these patients and thus no explanation or treatment is needed.
Two thirds of people with long COVID have symptoms of Ol and moderate to severe autonomic dysfunction. 11. 12 Ol has been labeled an epidemic since the mid-1990s and yet is still not well understood. 13 Given the burden long COVID places on economies as a mass-disabling event with high health care usage well beyond the acute illness phase, 14 it is pressing now more than ever to understand physiological mechanisms that contribute to Ol. Long COVID is a multisystem disorder with various manifestations in the immune, cardiopulmonary, and nervous systems. One finding is that Ol and long COVID share similar dysregulation in CBF, which may point to a shared pathogenesis. 15
Most people with OI develop symptoms after an acute viral illness or injury.1, 4 Since viral illnesses are the leading trigger of OI, it is unsurprising to the autonomic field that the COVID‐19 pandemic has caused an increase in cases of OI.6, 7 Long COVID, or the postacute sequelae of SARS‐CoV‐2 infection, describes people with chronic symptoms that persist following an acute infection of SARS‐CoV‐2.8 Symptoms of long COVID that overlap with OI include fatigue, dyspnea, headache, palpitations, and brain fog.9 According to the National Center for Health Statistics, the US Census Bureau, and the CDC, 6.8% of American adults are currently experiencing long COVID as of February 2024.10
Small fiber neuropathy in the post‐COVID condition and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical significance and diagnostic challenges - Azcue - 2025 - European Journal of Neurology - Wiley Online Library
PCC and ME/CFS patients demonstrated sensory SFN, as evidenced by impaired heat detection and increased tortuosity of small fibers in the central corneal subbasal plexus. The findings underscore the importance of a multimodal approach to comprehensively detect and characterize SFN. This study provides valuable scientific insights into the neuropathic manifestations associated with these conditions.
Does COVID increase the risk of Alzheimer’s disease?
Scientists discover that even mild COVID-19 can alter brain proteins linked to Alzheimer’s disease, potentially increasing dementia risk -raising urgent public health concerns.
The study found that individuals who had COVID-19 exhibited significant changes in brain biomarkers associated with Alzheimer’s disease. The Aẞ42:Aẞ40 ratio, a key marker of beta-amyloid buildup, was lower in COVID-19-positive participants compared to their matched controls. A reduced ratio of these proteins is commonly linked to Alzheimer’s pathology.
Strikingly, these biomarker changes were comparable to four years of aging or 60% of the effect size of inheriting a single APOE-4 allele, a well-known genetic risk factor for Alzheimer’s disease.
✾ On SARS-CoV-2 (COVID-19), brain damage, neurological damage, and dementia
Digital health app data reveals an effect of ovarian hormones on long COVID and myalgic encephalomyelitis symptoms | medRxiv
Background Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) disproportionately affect females, suggesting modulation by sex hormones. We sought to investigate whether symptom severity is influenced by changes in sex hormones over the menstrual cycle, or by hormonal contraception.
Interpretation Menstruation is associated with worsened symptoms in long COVID and ME/CFS. Users of combined hormonal contraception report a lower symptom burden than non-users, suggesting a modulatory role of ovarian hormones. These findings could empower menstruating people living with long COVID and ME/CFS to anticipate cyclical changes in symptoms and plan their activities accordingly, and could also inform their use of contraception.
Exertional Exhaustion (Post-Exertional Malaise, PEM) Evaluated by the Effects of Exercise on Cerebrospinal Fluid Metabolomics–Lipidomics and Serine Pathway in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
The elevation of serine in cerebrospinal fluid in ME/CFS was a key finding because of the many metabolic relationships that were uncovered. Elevated serine was associated with decreased 5MTHF, indicating disruption of one-carbon metabolism in the brain. This was supported by elevation in sarcosine, creatine, purines and thymidine derivatives. Energy metabolism was disrupted as indicated by elevated trans-aconitate.
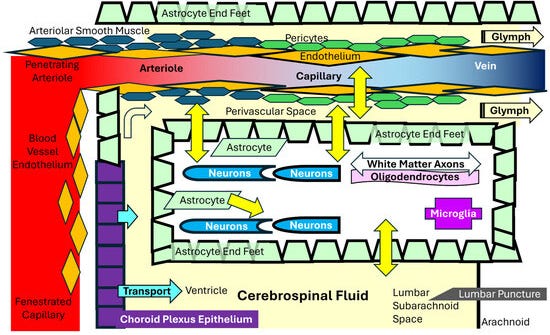
Choroid plexus volume is enlarged in long COVID and associated with cognitive and brain changes | Molecular Psychiatry
The present study provides novel evidence regarding the involvement of ChP in patients with post-COVID conditions. Importantly, ChP volume enlargement was associated with brain GM volume reduction and cognitive dysfunction, revealing a moderator role of the ChP volume between GM volume and cognition. Furthermore, ChP volume increment was associated with WM integrity and diffusivity alterations, increased functional connectivity, and immunological markers changes in PCC patients.
A study in Jordan found some Betacoronaviruses, including SARS-CoV-2 variants like Delta and Gamma, may carry prion-like proteins. These could explain links to neurological disorders and symptoms of long COVID.
In conclusion, the Q\N propensity scores might indicate the amyloid-forming potential or priogenicity of any short viral amino acid sequence and it can act as a regulator for viral infections and pathogenicity. It is proven that priogenicity can cause prion protein aggregation where the human body cannot get rid of. The findings of this study imply the high potential of Betacorona viruses to develop prions. One of the most important negative impact of prions is on the nervous system where any accumulation of prion protein in the astrocyte may lead to an acceleration in neurodegenerative diseases like Creutzfeldt-Jakob disease (CJD) and Scarpie
Depletion and Dysfunction of Dendritic Cells: Understanding SARS-CoV-2 Infection - PMC
As a bridge between innate immunity and adaptive immunity, DCs have important roles during virus invasion. The impaired function and reduced numbers of DCs are a catastrophe for the immune system during SARS-CoV-2 infection. The deficiency and dysfunction of DCs persist for several months after SARS-CoV-2 infection (113). Seven months after SARS-CoV-2 infection, the function of cDC2, as well as the number and IFNa production in pDCs, remains abnormal (113). This prolonged deficiency and dysfunction of DCs are associated with “post-acute COVID-19 syndrome” (”long-hauler syndrome”) in COVID-19 patients.